Become a Patreon!
Abstract
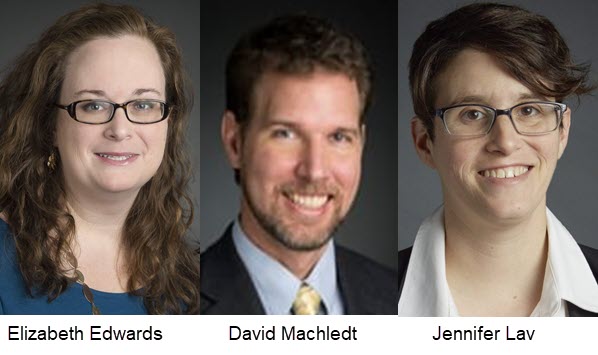
Excerpted From: Elizabeth Edwards, David Machledt, and Jennifer Lav, Retaining Medicaid Covid-19 Changes to Support Community Living, 14 Saint Louis University Journal of Health Law & Policy 391 (2021)(204 Footnotes) (Full Document)
COVID-19 has hit people with disabilities and their caregivers extremely hard. Morbidity and mortality rates for these individuals have been far higher than for the general population. The pandemic increased stress on the critical Medicaid home and community-based services (HCBS) system, which helps keep people in the community, rather than in institutions. Keeping people out of institutions has been especially important due to the high infection risk in many congregate settings. While the pandemic increased pressure on an already stressed HCBS system, associated Medicaid emergency-based flexibilities also drove some positive changes that facilitated access, shifted care away from congregate settings, and improved provider supports.
The federal and state COVID-19 responses have unfolded in the context of long-standing structural biases in Medicaid that favor institutional long-term care, undervalue HCBS for people with disabilities and the people who support them, and perpetuate health disparities, including racial/ethnic disparities. Chronic under-resourcing of HCBS presents complex challenges for its providers and participants who face an elevated risk of exposure, additional needs for personal protective equipment (PPE), and significant staff shortages. The federal response to COVID-19 has justifiably directed additional needed Medicaid resources and guidance toward nursing facilities devastated by the pandemic. However, HCBS provides alternatives to institutional services and needs comparable attention.
States have taken numerous emergency actions to stabilize HCBS provider availability, increase HCBS provider rates, and add new community-based services during the pandemic. Converting some of the more effective emergency measures into permanent policy changes could help diminish longstanding legal and administrative barriers that hinder access to Medicaid community-based services. A more robust and resilient community-based services infrastructure would allow people with disabilities to access the full benefits of community living both during and after an emergency. While some pandemic-based HCBS changes are appropriate only in the context of an emergency, evaluating the impact of those changes will help states respond to future emergencies.
This Article explores how the COVID-19 response has unfolded in the context of systemic inequities that have long hindered access to Medicaid HCBS. While some of the HCBS federal and state emergency policy changes have increased access to services and addressed longstanding barriers, others have likely exacerbated health inequities, particularly among Black, Indigenous, Asian American and Pacific Islander, and Latinx communities, and people with disabilities. This Article details the most common emergency changes that states have implemented to improve access to care and reduce transmission risk during the public health emergency. Finally, this Article discusses how states should evaluate the efficacy of these policies, including their impact on health equity, as they consider making some of the pandemic-based changes permanent--a step which could help reduce the long-standing institutional bias in Medicaid and help people with disabilities of all ages enjoy the full benefits of community living.
[. . .]
The long-term care system in the United States has long favored institutions over community-based programs. The COVID-19 pandemic perpetuated this bias in terms of funding, response, data gathering, and attention. Recent pandemic-based efforts to get people out of the hot zones of institutions and into community placements have not been matched with a commensurate push to support the HCBS programs needed by those individuals and their support systems.
States' COVID-19 responses have varied greatly. All took some advantage of available emergency authorities, but these actions supported some HCBS programs and services more than others. All of the changes that states made to their HCBS programs should be evaluated not only for their effectiveness in stabilizing HCBS programs during and potentially after the crisis, but also their effectiveness in reducing race- or disability-based disparities across the populations receiving services and the critical networks of HCBS providers and workers. Importantly, states must investigate who is benefiting, who is not, and whether these changes reduce or, conversely, worsen disparities in HCBS programs.
The COVID-19 changes to HCBS represent an important opportunity to strengthen HCBS programs as both more integrated and more equitable. That can only happen if states and advocates ask the important questions and listen carefully to both the individuals who benefitted from COVID-19-related changes, and to those who did not.
Elizabeth Edwards is a Senior Attorney at the National Health Law Program where she uses policy advocacy and litigation to improve access to community-based Medicaid services, ensure due process and the right to services, and address issues of bias in services.
David Machledt is a Senior Policy Analyst at the National Health Law Program.
Jennifer Lav is a Senior Attorney at the National Health Law Program.
Become a Patreon!


